While headaches and migraines are rare for most people, they can become far too common for others. Migraines affect up to 15 to 20% of the population at some point in their lives.
According to Dr. Gurneet Singh Sawhney, one of the best neurosurgeon in Mumbai, India, chronic headaches and migraines can be challenging to treat. And because there is no standard migraine treatment, physicians usually prescribe painkillers such as NSAIDs or opioids to relieve the pain.
While there is no single cure for chronic headaches, functional medicine can offer several therapies and treatments. Some medications can help prevent migraines and make them less painful. In conjunction with self-help remedies and lifestyle modifications, suitable medications may benefit.
Now, let’s understand,
What exactly is the difference between a headache and a migraine? And when does it become chronic?
A migraine is more than just a severe headache, as many people believe. A headache can be defined as any pain or pressure in your head on both sides, often caused by stress, muscle tension, or sinus pressure. They can lead to mild discomfort to severe pain and last for up to a week.
While the intensity and duration of the pain and pressure can vary, headaches are typically characterized by dull, throbbing pain. On the other hand, a migraine is always moderate to severe, with intense, pulsating pain. Other symptoms may include:
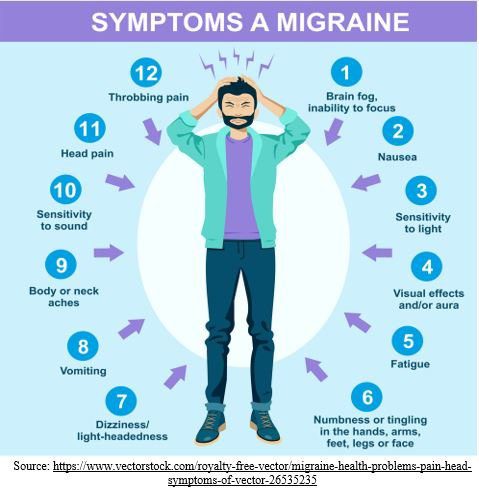
- Vomiting or nausea
- Pain behind the ear or in the eye
- Light, sound, or odour sensitivity
- Blind spots or temporary vision loss
- See floaters, flashing lights, or spots (usually before the migraine begins)
- Numbness or tingling on one side of the body in the face, lips, tongue, hands, or arms
- Weakness and dizziness
- Increase in migraine frequency over time
- Bowel habit changes
- Fatigue, unusual energy, frequent urination, or neck stiffness (before migraine episode)
- Aggravating pain with physical activity or exertion
Migraines are usually associated only with one side of the head. However, they can be equally aching on both sides or at the front or back of the head. According to the CDC, women are twice as likely as men to suffer from headaches and migraines, and they are most common in people aged 18 to 50.
To be diagnosed with chronic migraines, headaches must occur at least 15 days per month for more than three months, and 8 of those days must be migraines.
Let’s know,
What are the causes of migraines and headaches?
Headaches and migraines have the same risk factors. Headaches can result from muscle tension, sinus pressure, inflammation or pressure in and around the brain, infections, and traumatic brain injury.
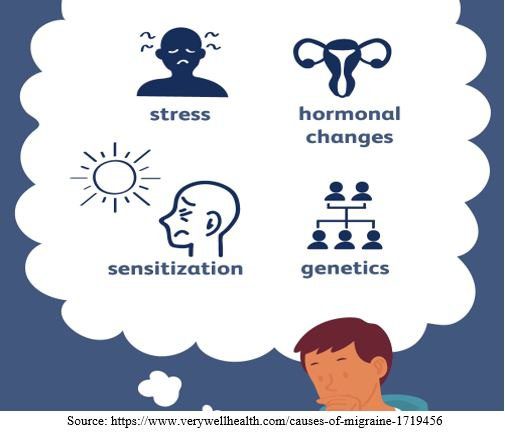
The precise cause of migraines is unknown because there does not appear to be a single cause. Migraines may have a genetic basis, but other internal and external factors can also cause them.
The following are well-known migraine risk factors:
- Anxiety, depression, and other mood disorders
- Pain disorders
- Stressful or distressing incidents
- Disrupted sleep patterns
- Injuries to the head or neck
- Overuse of medications
- Asthma
- Snoring
- Obesity
- Excess caffeine or alcohol intake
- Consuming certain foods or having irregular eating habits
- Chronic nausea
Environmental toxins and mould are two lesser-known causes of migraines and headaches. Unfortunately, exposure to both is possible wherever you go. According to one study, the average person has 91 toxins in their blood and urine because they come from many sources.
Toxins that cause headaches can be found in burning wood or gas, contaminated drinking water, cigarettes, lead, asbestos, and other chemicals.
Building water damage is a common source of toxic mould formation, which can sometimes go undetected. These toxins have been linked to inflammation, disease, and fatality. Another possible cause of brain problems and headaches is inflammation. Bacteria, infection, mould, toxins, gut dysfunction, and autoimmune diseases may cause inflammation.
Inflammation can spread to the brain from anywhere in the body, causing headaches. A leaky gut is a common source of this, leading to a leaky brain. Many gastrointestinal conditions such as IBS and celiac disease may cause headaches and migraines due to permeability and/or inflammation in the gut.
Another major potential cause of headaches and migraines is mitochondrial dysfunction. When our cells get unhealthy, a particular part of the cell that serves as the battery, mitochondria, becomes ineffective or impaired, resulting in the dysfunction of the affected cells. This may cause a chemical imbalance, dilated blood vessels, and inflammation, contributing to migraines.
What can I do when a headache or migraine attack occurs?
The cause of the headache determines the treatment for headaches. Rest and using heat, massaging, and muscle stretching can help ease or eliminate tension headaches, the most common type. Relaxation exercises, meditation, and other stress-reduction techniques may also benefit.
These methods and elevating the head and adequate fluid intake can help relieve sinus headaches. Of course, pain relievers and nonsteroidal anti-inflammatory drugs may benefit.
However, as previously stated, there is a limit to how much of these can be used. While some doctors may prescribe opioids to treat severe headaches, most believe that opioids cause more harm than good in the long term.
When it comes to migraines, many individuals discover that taking a pain reliever as soon as they notice symptoms can help prevent them from exacerbating. Typically, preventive medications are prescribed. Rest and therapeutic interventions for any co-occurring signs, such as nausea, are the best ways to get over it.
How can I reduce the occurrence of chronic headaches and migraines?
The first step is to identify your symptoms and start keeping a headache log to see if you have any obvious headache triggers.
Another critical step is to meet with a neurologist or neurosurgeon to discuss your health history. They can help determine any potential events or patterns that may be contributing to your headaches. Changes in your lifestyle may reduce the frequency of your headaches.
If you have one or more of the risk factors listed above, focus on improving your health in those areas, such as:
- Seeking assistance for underlying trauma, mood disorders, or high-stress levels.
- Establishing good sleep hygiene to get enough sleep regularly.
- Maintaining a healthy weight.
- Eating more nutritious foods.
- Avoiding trigger foods.
- Having an adequate amount of water.
- Establishing regular mealtimes or eating habits.
- Reducing or avoiding caffeine and alcohol consumption (if triggering).
- Getting snoring, allergies, and/or asthma under control.
- Seeking treatment and/or physical therapy for head or neck injuries.
- Addressing underlying conditions that cause nausea or pain.
- In women, regulating hormones lessens the severity of hormonal fluctuations.
Get tested if you have reduced the risk factors listed above and still aren’t feeling better.
Another option is to speak with your doctor about a possible mitochondrial dysfunction. Pulsed electromagnetic field (PEMF) therapy is an excellent treatment option for re-energizing cells and lowering the risk of migraines.
If you have noticed some digestive problems, consult Dr. Gurneet Singh Sawhney, a skilled neurosurgeon in Thane and Mumbai, to decrease inflammation, heal the gut lining, and incorporate supplements like magnesium as another option for relieving chronic headaches and migraines.
Visiting an experienced neurologist or neurosurgeon in Mumbai can help determine which risk factors you should focus on. Dr. Gurneet Singh Sawhney may discuss the medical history, run any necessary tests, and address any underlying disorders that contribute to your headaches or migraines.
Please get in touch with us if you or a family member suffers from chronic headaches or migraines. We would be glad to plan a consultation and develop a plan to help you achieve better health and headache relief!
