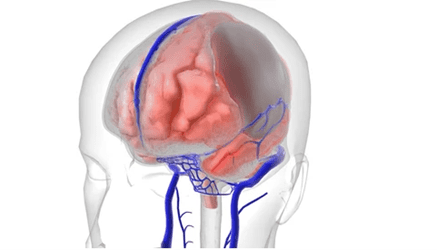
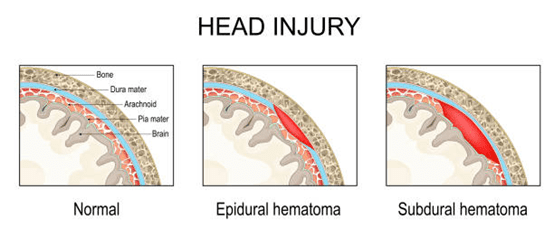
A frontoparietal subdural hematoma is a form of brain injury. In this condition, blood collects between the brain and its outer covering (dura mater) in the frontoparietal region. It often results from head trauma, leading to pressure on the brain. Globally, subdural hematomas account for about 20% of traumatic brain injuries.
According to Dr. Gurneet Singh Sawhney, an acclaimed neurosurgeon in Mumbai, India, “Early diagnosis and intervention are crucial in preventing long-term complications associated with frontoparietal subdural hematomas. Patients must be aware of the symptoms and seek immediate medical care if they suspect a problem.”
With over 18 years of experience, Dr. Gurneet Singh Sawhney specializes in treating complex neurological conditions, including brain subdural hematomas. He is highly regarded for his expertise in minimally invasive techniques, including endoscopic brain and neuroendovascular surgeries, which result in quick recovery and less scarring.
How Common Are Frontoparietal Subdural Hematomas?
Frontoparietal subdural hematomas are not as common as other types of traumatic brain injuries. However, they can occur in elderly patients or those who have suffered significant head trauma. Studies show that the frequency of subdural hematomas is more in older adults due to the brain shrinking with ageing, making it more vulnerable to injury.
In younger patients, brain subdural hematomas are generally related to more severe trauma, such as falls or vehicle accidents. Although not extremely common, the impact of these hematomas can be significant, affecting cognitive and physical abilities depending on the extent of brain compression and bleeding.
Symptoms of Frontoparietal Subdural Hematomas
The symptoms of a frontoparietal hematoma can vary depending on its severity and the pressure it places on the brain. Common symptoms include:
- Persistent or worsening headaches
- Nausea and vomiting
- Dizziness and confusion
- Weakness or numbness in limbs
- Difficulty with speech or vision
- Seizures
- Blurred vision
- Cognitive changes or memory issues
- Loss of consciousness in severe cases
If left untreated, this condition may cause permanent brain damage, emphasizing the importance of early diagnosis.
Causes and Risk Factors for Frontoparietal Subdural Hematoma
- Head Trauma: The most common cause of frontoparietal hematomas, usually due to accidents or falls.
- Age: Older adults are at higher risk due to brain atrophy, which increases the chance of blood vessel rupture.
- Blood Thinners: Patients on anticoagulants are at a higher risk due to increased bleeding tendencies.
- Alcohol Abuse: Chronic alcohol consumption weakens blood vessels and increases fall risk. It can also cause brain tissue shrinkage, increasing the risk of hematomas after head injuries.
- Previous Brain Injury: A history of head trauma makes patients more susceptible to future hematomas.
In some instances, even mild trauma can result in a subdural hematoma if the brain shifts inside the skull, causing blood vessels to stretch and tear.
Recognizing these risk factors can help take preventive measures or seek early intervention.
How is Frontoparietal Subdural Hematoma Diagnosed?
Diagnosing a frontoparietal hematoma requires comprehensive clinical evaluation and imaging tests:
Neurological Exam: Doctors assess cognitive function, coordination, and reflexes to determine brain damage.
CT Scan: A common imaging method that identifies the presence and size of a hematoma.
MRI: Provides more detailed imaging of soft tissues to evaluate the extent of the injury.
Angiogram: A specialized test to visualize blood vessels and detect bleeding points.
Early and accurate diagnosis is vital to determine the best treatment plan and prevent further complications.
Treatment for Frontoparietal Subdural Hematoma
“The treatment of frontoparietal subdural hematomas depends on the size, location, and severity of the bleeding and the patient’s overall health,” explains Dr. Gurneet Singh Sawhney. For significant hematomas that pose a threat to brain function, surgery is often necessary to relieve pressure on the brain and prevent severe complications. Here are the primary treatment options:
Burr Hole Drainage
This minimally invasive procedure involves drilling small holes into the skull to drain the collected blood. It is usually performed for smaller, less complicated hematomas.
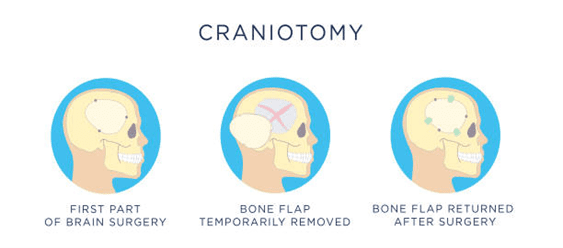
In cases of larger or more severe hematomas, neurosurgeons often perform craniotomy. This involves removing a portion of the skull to access and remove the clot. Once the hematoma is cleared, the skull is replaced.
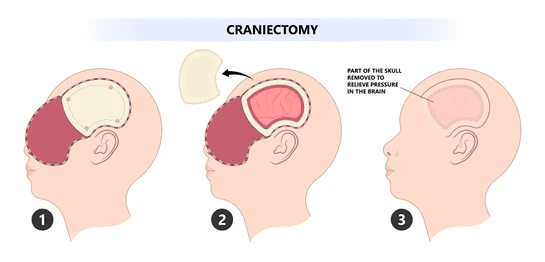
Decompressive Craniectomy
This procedure is reserved for life-threatening cases when the brain is under significant pressure due to swelling. It involves removing part of the skull to relieve pressure and allow the brain to expand.
Endovascular emobilization:
Endovascular embolization is a treatment that may be considered for frontoparietal subdural hematomas when the bleeding is caused by or associated with a vascular abnormality, such as an aneurysm or an arteriovenous malformation (AVM). In cases where a subdural hematoma is secondary to these vascular issues, endovascular embolization can help control the source of the bleeding. The procedure involves inserting a catheter through a blood vessel, typically in the groin, and guiding it to the affected brain region. Once in place, embolic agents (such as coils, particles, or glue) are delivered to block the abnormal blood vessels, stopping the hemorrhage and preventing further bleeding. This technique can be crucial for stabilizing patients and preventing additional brain damage.
Non-Surgical Treatment
For small hematomas or patients unable to undergo surgery, close observation and medical management may be sufficient. However, this option is rare and requires careful monitoring for any changes.
Recovering from a Frontoparietal Subdural Hematoma
Recovery from a subdural hematoma can vary depending on the severity of the injury and the treatment approach. For patients who have undergone surgical procedures like craniotomy or Burr hole drainage, the initial phase of recovery usually involves a stay in the hospital for monitoring neurological functions and post-surgical complications, such as swelling or infection. Regular imaging scans ensure the hematoma has been successfully removed and brain pressure is stabilized during this time.
Once discharged, rehabilitation plays a crucial role in full recovery. If the hematoma affects movement, patients may require physical therapy to regain motor skills and coordination. Cognitive rehabilitation might also be needed to address memory or speech issues that can result from brain injuries. Recovery time can vary from a few weeks to several months, depending on the individual case and the extent of brain damage.
Routine follow-up with a neuro specialist is essential to monitor progress and prevent recurrence. Lifestyle modifications, such as avoiding strenuous activities or controlling blood pressure, may be recommended to support long-term recovery.
Conclusion
Frontoparietal subdural hematomas can be life-threatening if not diagnosed and treated promptly. Patients can achieve optimal recovery with proper care from specialists like Dr. Gurneet Singh Sawhney, who has extensive experience managing such cases with precision and care, ensuring the best possible patient outcomes.
FAQ
1. What is the life expectancy after subdural hematoma?
2. What is the patient's condition with frontoparietal subdural hematoma 2 months later?
3. Is there subdural hematoma treatment without surgery?
4. Can frontoparietal subdural hemorrhage heal itself?
5. Is a subdural hematoma the same as a stroke?
Reference links:
https://my.clevelandclinic.org/health/diseases/21183-subdural-hematoma
https://www.webmd.com/brain/subdural-hematoma-symptoms-causes-treatments
Disclaimer: This page is intended for informational and educational purposes and not for promotional use.